Pigment spots are a common concern in dermatology. These skin abnormalities, often called hyperpigmentation, result from excessive production of melanin, the pigment responsible for skin color.
Various factors can disrupt the natural synthesis of melanin, leading to an overproduction of this pigment. Brown spots, or hyperpigmented spots, can appear after excessive exposure to the sun and sunburn, during hormonal changes such as during pregnancy, after skin inflammation, or following minor skin trauma such as on some post-acne scars. The risk of hyperpigmentation increases with age.
These spots can be more or less dark, more or less extensive , and affect all skin types, with a more marked incidence in individuals with dark skin phototypes.
Solar lentigo (age spots)
Solar lentigo, also known as senile lentigo or age spot, is a common form of skin hyperpigmentation characterized by well-circumscribed, flattened spots, typically 1 to 3 cm in diameter. These hyperpigmented spots result from a localized increase in melanin production by melanocytes, often in response to years of cumulative exposure to the sun's ultraviolet (UV) rays.
Solar lentigines can vary in appearance, ranging in color from light brown to dark brown. The texture of these spots is usually smooth, and they do not cause any palpable changes to the surface of the skin. These spots most often appear on areas of the skin that are frequently exposed to the sun, including the face, hands, forearms, chest, back, and shins. These areas receive regular sun exposure, which is why they are more susceptible to UV damage.
The appearance of solar lentigines is mainly triggered by acute and chronic exposure to UV rays. Sunlight causes cumulative damage to the DNA of skin cells and impairs cellular repair mechanisms, leading to excessive melanin production in specific areas. Natural skin aging, or senescence, also plays a significant role in the development of these spots. With age, the skin's ability to repair UV damage decreases, which promotes the appearance of lentigines.
Therefore, to prevent these spots it is crucial to use sunscreen daily to protect the skin from the harmful effects of the sun.
Post-inflammatory hyperpigmentation
Post-inflammatory hyperpigmentation ( PIH ) manifests as irregular, flattened, heavily pigmented spots or plaques. These marks typically appear at sites of previous injury or inflammation. PIH can persist for months to years, depending on the severity of the initial inflammation and the skin's ability to regenerate.
The color of the areas affected by HPI can range from light brown to dark brown, and in some cases, it can even take on gray/blue-black hues if the dermis, the deeper layer of the skin, is affected. This color variation is due to the depth and intensity of the melanin accumulated in the skin. Melanocytes, the cells responsible for producing melanin, increase their activity in response to inflammation, thus producing an excess amount of pigment.
Acne scars represent one of the most common examples of post-inflammatory hyperpigmentation. Severe or repeated breakouts cause inflammation that stimulates melanocytes to produce more melanin. Similarly, burns, cuts, and surgical procedures can cause PIH by disrupting the integrity of the skin and triggering an inflammatory response.
Several factors can influence the severity and duration of PIH. People with darker skin are generally more likely to develop post-inflammatory hyperpigmentation due to the presence of more active melanocytes. Additionally, repeated exposure to UV rays can exacerbate pigmentation by further stimulating melanocytes.
To prevent post-inflammatory hyperpigmentation, using sunscreen to protect the skin from UV rays is essential to prevent worsening of pigmentation.
Melasma
Melasma manifests as areas of skin with persistent, non-scaly, flattened hyperpigmentation . The color of these areas ranges from light brown to gray/bluish, depending on the depth of the affected skin compartments, ranging from the epidermis to the dermis. These patches appear primarily on sun-exposed areas of the skin, such as the face and forearms. Melasma patterns are often bilateral, presenting in one of three distinct patterns: centrofacial (affecting the forehead, nose, cheeks, and upper lip), malar (affecting the cheeks and nose), or mandibular (affecting the jaw).
The main triggers of melasma include chronic sun exposure, which is the most significant factor, accounting for 40 to 44% of those affected. Ultraviolet light stimulates melanocytes to produce an excessive amount of melanin, leading to the formation of dark spots. In addition, hormonal fluctuations, such as those observed during pregnancy or due to the use of hormonal contraceptives, can trigger or worsen melasma. This condition is often called "pregnancy mask" when it occurs in pregnant women.
Genetic predisposition also plays a crucial role in the development of melasma. Family history increases the risk, suggesting a hereditary component in susceptibility to this condition. Additionally, skin inflammation and aggressive cosmetic treatments can exacerbate melasma by causing an inflammatory response that further stimulates melanin production.
How to treat pigment spots?
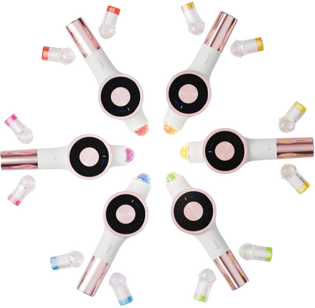
Lightinderm's SPOTLESS program offers a complete solution to treat hyperpigmentation by activating the skin's natural processes of melanin elimination and limiting its excessive production. This treatment works in several phases to effectively combat the hyperproduction of melanin and therefore the appearance of pigment spots.
Here are the three light + photo-active synergies that make SPOTLESS a powerful ally against hyperpigmentation: